The Darker Side of
Supplementing Vitamin D
(A Comprehensive Research Analysis on Why Excess Supplementation is Often a Cause of Disease More Than a Cure)
by Rick Fischer C.H.H.C., h.T.M.A.P.
May 2016

As a leading researcher and educator in the field of mineral-based health, this 2016 article by Rick Fischer stands as one of the original and most comprehensive works written that speaks out against the incorrect use (and over-prescribing) of Vitamin D supplementation. In the years since this article was written, more and more science is coming out that validates ("discovers!") the concepts originally warned about herein. (We also provide an even deeper education on Vitamin D and its interrelationship with minerals and health within the Mineral Mastery nutrition program).
Like most people, I used to be a strong believer in the benefits of supplementing Vitamin D... until I became heavily involved in the field of nutritional research and then subsequently seeing first hand in clinical practice just how dangerous this "fad supplement" can be, especially long-term taken incorrectly as many people are doing. Like most, I had been conditioned to believe, through what doctors, nutritionists, and endless online articles tell us, that supplementing lots of Vitamin D is both harmless and important, especially as it's the "sun vitamin". It's hyped in health and medical articles as being a cure for almost everything under the sun. This conditioning runs so deep that most people then roll their eyes if one dares to suggest otherwise.
To be very clear, and before any reader jumps to an assumption by the title of this article, it's acknowledged that Vitamin D itself absolutely has health benefits. We all need it. This is not the issue, and there is plenty of literature and research that supports the importance of Vitamin D. So let's make it clear from the start that Vitamin D itself is important - optimizing your Vitamin D level has many benefits, including providing immune support. The issue however, is thinking that taking it in pill form (the way it's widely promoted) is a safe way to raise one's level, and without consequences, especially when taken long term, at higher doses, and without other cofactors as is so often promoted or prescribed.
This brings up the dark history that has led to today's widespread over-promotion of Vitamin D, along with the dangerous side to Vitamin D supplementation that very few talk about. This article aims to advance the understanding for both public and practitioners, bringing this deeply researched area to light as one of the original, comprehensive discussion articles on the topic.

Incorrectly supplementing Vitamin D pills (especially at higher dose) could be putting millions of people at risk.
To begin, few people differentiate between sunlight Vitamin D and pill-form Vitamin D; they simply and erroneously assume they are equal. Nor do people make the connection to a symptom that arises years later back to a supplement they took years before. Nor are they educated on the basic interrelationship between vitamins and minerals. This mineral interrelationship is almost all but completely ignored in medical school, yet is at the very foundation of our health. When one comes to understand the effect that excess Vitamin D in supplementation form has on long term health and the body's mineral system (as explained herein), we then begin to see its more dangerous side. The truth is, the recent herd mentality fad of blindly pushing Vitamin D supplements is putting millions of people at high risk for everything from weight gain and heart attack to decreased energy, increased depression, and even future pathological disease processes. The National Academies of Sciences, Engineering, and Medicine stated back in 2010 that:
"Signals suggest there are greater risks of death and chronic disease associated with long-term high vitamin D intake". [source]
Chances are, if you're popping vitamin D pills, while it may help in the short-term, long-term it may be putting your health at risk, as explained within this article.
"Healthy people have been popping these pills, but they should not continue taking vitamin D supplements unchecked. At a certain point, more vitamin D no longer confers any survival benefit, so taking these expensive supplements is at best a waste of money."
~Muhammad Amer, M.D., M.H.S (lead researcher at John Hopkins)
Oral Vitamin D supplementation is an immunosuppressive steroid and acts differently from sunshine Vitamin D!
First, it's important to understand that the Vitamin D we get from the sun (which is in a sulfate form) affects the body differently from isolated synthetic oral Vitamin D supplementation. What I'll be referring to in this article is oral Vitamin D supplementation...which really, isn't even a vitamin, but an immunosuppressive steroid[1]! When we're exposed to the sun (UVB), the skin synthesizes Vitamin D sulfate. This sulfate form is water soluble, is able to travel freely in the blood stream, strengthens the immune system, protects against cardiovascular disease, helps against depression, assists with detoxification, and nourishes the brain. Sunshine Vitamin D therefore really is healthy for us, as long as we maintain intelligent exposure.
The supplement form of Vitamin D3 however is un-sulfated, not water soluble, and requires LDL ('bad cholesterol') to be transported. The un-sulfated supplement form does not offer the same benefits as the sulfate form, although the supplement form is great at transporting calcium through the body which the sunshine form doesn't do - at least, not initially. The sulfated form, after offering its other benefits in the body, 'drops' the sulfate and then, in its newly un-sulfated form, is able to assist with calcium and bone health. So basically, the sunshine version offers the best of both worlds, whereas the supplement version misses out on a lot of the benefits…and…as you'll learn in this article, comes with consequences. Specifically, incorrectly supplementing too much Vitamin D may lower Potassium and Vitamin A, lowers Magnesium, and tends to raise Calcium. Let's look at the implications of this.

Magnesium activates Vitamin D, and considering that most people are deficient in magnesium, much of the Vitamin D we're supplementing remains inactive.
The balance between Calcium and Potassium affects thyroid expression. The higher this ratio, the slower the thyroid (or the more one may begin experiencing symptoms associated with hypothyroid even if, clinically, the thyroid still appears fine. As the Ca/K ratio increases, this impairs cellular sensitization to thyroid hormone while also impairing cell permeability of hormones and nutrients, leading to a slowing effect of the thyroid, and potentially, weight gain!
Another consequence of low Potassium as a result of excessive Vitamin D supplementation is a higher Sodium to Potassium ratio. As the Na/K ratio increases, inflammation and the stress response increase. As one's stress increases, Magnesium drops. In other words, taking excessive Vitamin D leads to magnesium depletion. Magnesium is also used up in the conversion of Vitamin D into its active form...again the more Vitamin D a person is popping, the more they're depleting their magnesium stores. Magnesium deficiency in turn leads to increased risk for heart attack, especially in the face of high stress and a high Calcium level. The lowered Magnesium also contributes to diabetes (as Magnesium helps regulate insulin). The consequences of high calcium relative to low magnesium also lead not only to psychological concerns and heightened anxiety, but also unstable blood sugar levels.
The irony is magnesium is needed to activate and raise Vitamin D, and considering that most of the population is deficient in magnesium, much of the Vitamin D we're being told to supplement remains inactive. Plus, by taking all this vitamin D in supplement form without adequate Vitamin K2 (a key factor in Vitamin D's safety as will be discussed throughout this article) we're only lowering magnesium further and impairing the goal of raising Vitamin D! If you really want to raise your body's natural vitamin D level, work on boosting your magnesium - it's a key cofactor required to bind Vitamin D to its transport protein.
Vitamin A helps decrease inflammation. However Vitamin D antagonizes Vitamin A. Vitamin A deficiency also impairs iron utilization and transport, and it's well known that Vitamin A deficiency is a cause of iron anemia[3]. Taking synthetic Vitamin D, by lowering Vitamin A, could therefore contribute to such anemia.
Both Magnesium and Potassium are necessary for the body's anti-inflammatory response, and yet, as we've already looked at, Vitamin D lowers both of these essential minerals. Without the necessary anti-inflammatory response, a host of disease processes arise, and arteries also become damaged. Calcium and cholesterol then get drawn to these sites of arterial damage and plaque builds up, leading to atherosclerosis (hardening of the arteries). This is why it's so essential to be taking Vitamin K2 when you're supplementing Vitamin D, since K2 helps keep calcium in bone where it needs to be. Countless people are led to believe that they can simply supplement Vitamin D alone, and are often even told to do so by their doctors or practitioners. They are rarely if ever taught about the increased importance of addressing magnesium, potassium, Vitamin A and especially K2 when supplementing D! This is of the utmost importance, and is the primary key that allows some people to supplement Vit D at higher doses without consequences!
Too much vitamin D by itself is not only toxic, but also contributes to soft tissue calcification...especially when taken without enough Vitamin A and K2. It is those other two nutrients that must also be taken with Vitamin D to avert the affect of tissue calcification, and which allow for higher doses of Vitamin D supplementation to be safely tolerated. This is typically ignored when people are just told to "take Vitamin D". Furthermore, Vitamin A (true Vitamin A in retinol form) is necessary for the binding of copper onto the protein ceruloplasmin which makes copper bio-available (and in turn supports iron). Since Vitamin D can lower Vitamin A which lowers ceruloplasmin, this can then contribute to copper bio-UNavailability. This in turn leads to many of the negative side effects associated with copper imbalance, while also raising bio-unavailable calcium - weakening the bone matrix and contributing to a higher risk of osteoporosis. Yes, contrary to the lies we're told by Vitamin D proponents, too much Vitamin D at best has a negligible effect on bone density or, as has also been shown, may actually increase the risk of bone loss and osteoporosis, not to mention increase the risk of kidney stones[1]!
"Until now we haven’t worried about giving people extra vitamin D because we thought "it might help anyway and of course (as it’s a vitamin) doesn’t do you any harm". With our increasing knowledge, we should now know better….
One 2015 randomized study of 409 elderly people in Finland suggested that vitamin D failed to offer any benefits compared to placebo or exercise - and that fracture rates were, in fact, slightly higher……
One study involving over 2,000 elderly Australians, which was largely ignored at the time, and the one just published found that patients given high doses of vitamin D or those on lower doses that increased vitamin D blood levels within the optimal range (as defined by bone specialists) had a 20-30% increased rate of fractures and falls compared to those on low doses or who failed to reach "optimal blood levels".
~ Tim Spector, Prof of Genetic Epidemiology [2]
Learn more about all these interactions between minerals and vitamins and how they influence health and symptoms... in Mineral Mastery!
Cholecalciferol can lead to hypercalcemia
Returning to the issue of soft tissue calcification, the Merck Veterinary Manual says the following about Cholecalciferol (which is essentially Vitamin D, used as a rat poison)... "Cholecalciferol produces hypercalcemia, which results in systemic calcification of soft tissue, leading to renal failure, cardiac abnormalities, hypertension, CNS depression, and GI upset." Sure, this is relating to effects in rodents, and it is known that cholecalciferol acts differently on rats (where it does have a toxic quality) than it does on humans. Nonetheless, it still conveys (and does not discount) the fact that too much vitamin D can lead to hypercalcemia and calcification - not ideal! Once again though, there are studies that show high dose Vitamin D supplementation creating hypercalcemia in one person but yet not in another, and then the argument is made that this connection to hypercalcemia is nothing more than fear-mongering.
Why then do some people feel good when taking Vitamin D pills? There are a few reasons. For one, the effect is often a short term benefit at the expense of detrimental effects longer term (more on this in a moment). For some people, taking Vitamin D supplementation can be beneficial - typically the fast metabolizer with high potassium. This mineral pattern is best reflected through a Hair Tissue Mineral Analysis (HTMA). Blood testing for this purpose is quite inadequate as blood serum levels can fluctuate day to day and do not accurately represent stored tissue mineral levels. Through HTMA testing we can see if a person is a fast metabolizer (as generally defined when the Calcium to Phosphorus ratio is below 2.6 and with lower calcium relative to sodium and potassium) or a slow metabolizer (when the Ca/P ratio is above 2.6 and with higher calcium relative to lower sodium and potassium).
Roughly 80% of the population are slow metabolizers, and for these people, who generally already have higher levels of calcium and lower levels of potassium, Vitamin D supplementation can have adverse affects, especially when they're ignoring Vitamins A and K and minerals such as magnesium and potassium. Fast metabolizers may benefit more from Vitamin D supplementation as it can help bring better balance to their mineral pattern. As has already been stated a few times in this article, Vitamin D supplementation is also safer when adequate Vitamin A, K2, potassium and magnesium are taken alongside. This is often where most people error, as they are taking lots of Vit D, but ignoring those other key nutrients.
Another important yet often overlooked consideration is the reason why people say they 'feel good' taking Vitamin D... could it be Vitamin D's immunosuppressive effect?
"As the immune system becomes increasingly inhibited, fewer L-form bacteria are killed. Furthermore, the Vitamin D Receptor is no longer able to transcribe the antimicrobial peptides, and fewer bacteria are killed by DNA fragmentation. As fewer bacteria die, fewer inflammatory cytokines are released, and fewer toxins and cellular debris enter the bloodstream. As the level of inflammation temporarily decreases, a patient will start to feel better....
...Naturally, such patients feel that the extra vitamin D is helpful. It may take decades before their L-form bacterial load rises to the threshold at which they are diagnosed with an autoimmune illness, or have a stroke or heart attack. At this point later in life, they seldom make the connection between their current illness and the extra vitamin D they have been taking with no apparent ill effect for such a long period of time."
~Amy Proal, PhD
Further evidence of the immunosuppressive effect leading to "short-term benefit" is explained by Shoenfeld and Gershwin (2009) in the Annals of the New York Academy of Sciences, Volume 1173. Contemporary Challenges in Autoimmunity:
" ...vitamin D supplementation, if it achieves high enough levels of the precursor forms (vitamin D and 25-D), actually contributes to VDR blockage and a decrease in the innate immune response. ...at high levels 25-D and 1,25-D can displace the natural ligans from nuclear receptors, such as the thyroid-α-l, adrenal, and glucocorticoid receptors. This displacement appears to have the potential to disrupt the endocrine system. It could also lead to immunosupression by reducing the ability of these receptors to induce production of antimicrobial peptides. Thus, at least two mechanisms exist by which vitamin D supplementation could suppress innate immune system function. This suppression would lead to short-term improvements in patients taking higher levels of vitamin D by slowing bacterial death and subsequent immunopatholigical reactions. Therefore, studies that evaluate the role of vitamin D supplementation in chronic inflammatory diseases should take into account the potential for short-term symptom reduction as well as exacerbation of the disease process over the long term from pathogen increase." [12]
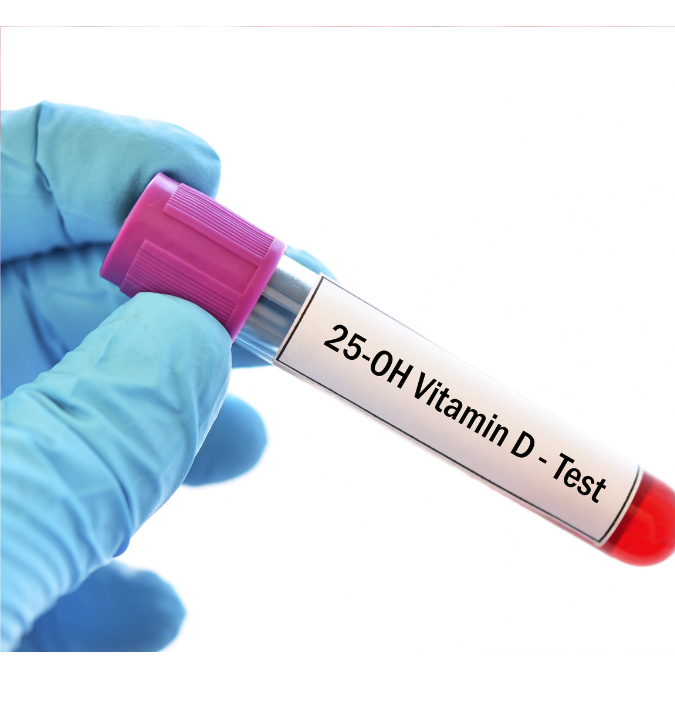
Very few doctors test for both the storage AND active form of Vitamin D, increasing the appearance of widespread deficiency.
What about those serum tests that show almost everyone being deficient in Vitamin D? There's a good chance your doctor has told you that you're low in Vitamin D. One problem with these tests is that your typical blood test (along with most studies which rely on blood) most often looks only at Vitamin D in the form of 25(OH)D (the storage form of D). This level usually tests low. However there is also the active (calcitriol) form (1,25(OH)2 D3) - very few doctors ever test for this. If doctors test both forms as opposed to just one, they would see that Vitamin D deficiency may be less extreme than what it appears to be. If your doctor is telling you that you're low in Vitamin D, demand that s/he first test BOTH the storage and active forms to give you a more accurate picture.
Added to this, most people will still be deemed Vitamin D insufficient when their results come back between 21-29 ng/mL even though those levels have traditionally been considered a normal, healthy level! The National Academy of Medicine for example, (formerly the Institute of Medicine), states that 97.5% of people with 25(OH)D levels >20 ng/mL have adequate vitamin D for bone health, yet many prescribing physicians tell their patients with such levels that they are 'deficient', and they then push the idea that more supplementation is necessary. Yet, too much Vitamin D can be just as dangerous as too little.
"adequate vitamin D prevents heart disease, but too much vitamin D promotes heart disease. The available evidence suggests that the lowest risk of heart disease occurs when vitamin D status is between 20 and 40 ng/mL." [4]
Furthermore, In 2006, the Merck Manual listed 25–40 ng/ml as the normal 25(OH)D range.[5]
This healthy range, and not pushing for higher levels, is further verified by the Institute of Medicine in their comprehensive review and report published in 2010, stating:
"Higher levels have not been shown to confer greater benefits, and in fact, they have been linked to other health problems, challenging the concept that 'more is better.'" [6]
The message that "everyone is deficient" became a monetary windfall for testing labs
So why are people today led to believe that supplementing at high doses is fine and harmless? Well, it's partly due to what could be considered misinterpretation of a few studies in the early 2000s, together with a report by the Endocrine Society put out in 2011, just a few months after all the extensive research and findings by the aforementioned Institute of Medicine had been published. This new report was a complete contradiction to all the previous findings by the Institute of Medicine that most people had sufficient Vitamin D, and instead pushed the idea that most people were instead deficient. This led to a massive increase in both testing for Vitamin D deficiency, as well as supplement sales. This new report however was led by a medical doctor renowned for his pushing of Vitamin D (who, with an obvious conflict of interest, has received many thousands of dollars from labs and pharmaceutical companies tied to Vitamin D testing and supplements).
This new message that "everyone is deficient" became a monetary windfall for testing labs, with Vitamin D testing now being the 5th most common lab test covered by Medicare. In fact, between 2007 to 2016, the increase in doctor-ordered lab testing of Vitamin D for Medicare patients has increased 547%!
Not only that, but laboratories appear to be using cut-points that are much higher than the committee tasked by the Institute of Medicine suggested is appropriate [6], naturally leading more people to be diagnosed as "deficient".
Practitioners who focus only on the blood level of minerals are less likely to see the mineral effects of excessive Vitamin D, with the exception perhaps of extreme Vit D doses causing hypercalcemia. Even many HTMA practitioners still have not caught on, especially when the assumption is made that an HTMA chart can be read at face value (which it should not) and expecting a straight correlation that taking Vitamin D will, in all cases, cause the same mineral pattern to appear in a chart. Such thinking ignores the myriad of other factors that also influence a person's mineral profile. For example, while Vitamin D without magnesium or K2 can increase tissue calcium, I've seen some who argue that all the high-dose Vitamin D they're giving to their patients is harmless simply because they don't see the HTMA calcium level increasing. Of course, HTMA calcium doesn't move solely as a result of supplementation, but as just mentioned can be influenced by various other factors, including even just one's stress response. Meanwhile, I've had clients come to me who've been taking 5000iu, 10,000iu, or more of Vitamin D daily as per their practitioner's guidance, with years of historic HTMA chart data to reference, and their potassium levels progressively have gotten worse over the years along with very little improvement in symptoms.
In the end, popping back all this extra D supplementation without further inquiry is today opening the door to a much wider range of health conditions...conditions that may take years to appear. There is even 'a wealth of evidence supporting the hypothesis that significant consumption of oral Vitamin D among the young is a risk factor for inducing celiac disease' [7].

"The definition of Vitamin D deficiency needs re-evaluation in view of the fact that low 25(OH)D is found in both healthy and sick individuals... It is reasoned that if low 25(OH)D indicates a current or potential disease state, then increasing 25(OH)D by supplementing with vitamin D should provide some symptom relief and/or protection. So far, there is scant evidence for this hypothesis... Despite the recent increase in vitamin D supplementation, chronic diseases have increased & are expected to continue increasing." [8]
"The evidence shows taking extra vitamin D doesn’t help for a number of conditions for which it’s prescribed, most people get enough, and over-use may actually be harmful. ~[15]
"Taking extra calcium and/or vitamin D without an understanding of how they are interrelated with other vital nutrient minerals can start a cascade of adverse changes in the nutrient mineral system. Unfortunately, for countless numbers of people, their medical doctors lack this essential information and understanding of dynamic scientific nutrition."
~Dr. Rick Malter, Ph.D. [4]
Compromised kidney function can also contribute to low Vitamin D
It is shocking and disheartening to see the number of physicians, nutritionists, and other practitioners telling their patients to boost their Vitamin D levels based on (a) not testing both active and storage forms, (b) telling patients they are insufficient when indeed they may not be, (c) not assessing other cofactors (such as magnesium) necessary to maintain an adequate D level, (d) suggesting dosages ranging from 5000iu to 50,000iu, (e) looking only at short-term benefit without consideration for longer term pathological processes, and (f) not considering (or educating their patients on) the increased need for Vitamin K2, Vitamin A, Potassium and Magnesium when supplementing such high doses! Furthermore, how often is the mineral boron considered? Rarely. Yet, a deficiency of boron can also accentuate a Vitamin D deficiency, and so boron may also be supportive for people with low Vitamin D.
Then, these practitioners who are pushing more Vitamin D on people, are they considering kidney function? It's the kidneys that play a major role converting Vitamin D (whether from the sun or supplements) into the active form. Compromised kidney function can therefore also contribute to low Vitamin D. The point is, if your Vitamin D is low, it shouldn't be an automatic assumption that you need to supplement more D, but rather should raise the inquiry into what OTHER imbalance is occurring which in turn is affecting Vitamin D status.
Likewise, those with oxalate issues, or a history of kidney oxalate stones, also need to be more careful with supplementing Vitamin D (especially at higher doses), as doing so could increase urinary calcium and further contribute to stone formation. Just because one person is able to take high dose Vitamin D without consequences does not automatically mean that doing so is safe for everyone. Bio-individual factors, so often overlooked when a one-size-fits-all supplement or program gets promoted, must be considered!
Before you waste money on supplementing synthetic Vitamin D, it's so important that you first understand the risks of doing so and how it can affect your mineral ratios and your body's health in the long term. Even something as "popular" as a Vitamin D pill can have very serious consequences on health when used improperly. Unfortunately, until HTMA is more widely adopted by mainstream health, until bio-individuality is considered, and until educational training such as that offered through www.MineralMastery.com is more widely taught, these effects will largely go hidden and denied, while doctors and nutritionists alike will continue to tout Vitamin D supplementation as a cure-all for everything, not aware of the downstream effects.
"Studies which incorrectly interpret the reason for low vitamin D in patients with chronic disease have been seized upon by the media, and form the basis of massive advertising campaigns – which, along with ill-informed recommendations by doctors and researchers, have created a perfect storm of misunderstanding and bad advice."
~Amy Proal, Ph.D.
Supplementing Vitamin D on a temporary basis to provide short-term immune benefit can be okay and may be well warranted, but most people are taking Vitamin D (often at high doses) on an ongoing basis for months or years. The benefits of taking vitamin D are usually short term, and most studies only track this short-term period. This is why many so-called 'experts' continue to promote the benefits of taking more vitamin D, not understanding the potential for negative longer term effects.
"One of the abiding weaknesses of studies on the effects of vitamin D on health is that researchers simply do not follow subjects consuming the secosteroid for a sufficient period of time. Instead, they tend to track subjects over the course of weeks, months, or one or two years, during the period of time when study participants are usually feeling the palliative effects of the steroid. This practice is a mistake as it does not account for the long-term immunosuppressive effects." [9]
If you're concerned about your Vitamin D levels and want to raise it in a safe way, there are natural ways to do this which are far safer than taking synthetic supplementation. First and foremost, check your magnesium level!! You can pop all the Vitamin D in the world, but without adequate magnesium you will still have trouble raising your D levels. This is even more true when we consider that most of the Western world is over-calcified, and as a natural feedback loop the body attempts to lower Vitamin D as a result (to prevent calcium from going higher). As Dr. Jack Kruse explains:
"It is physiologically impossible to have a 25(OH) blood test (“Storage-D”) to be less than 35 ng/dl and a Magnesium RBC level to be above 6.5mg/dL because of the negative feedback tied to calcium levels." ~Dr Jack Kruse
Vitamin K2 should always be considered when supplementing Vitamin D.
Taking isolated Vitamin D pills therefore is not the answer, as it only compounds the calcification issue, which then further depletes magnesium, in turn promoting the body's need to suppress Vitamin D. In other words, if you truly are Vitamin D deficient, chances are it may be because you are deficient in magnesium and/or over-calcified! As well, since magnesium is a necessary cofactor for Vitamin D, the very nature of taking Vitamin D supplements means you are using up your body's precious stores of magnesium... which then circles back to compounding the calcification issue! This calcification issue can be mitigated by taking adequate Vitamin K2 along with the Vit D.
Vitamin K2 is needed to support 2 proteins, Matrix GLA Protein and Osteocalcin. These proteins are at the core of keeping bones strong (especially Osteocalcin) and preventing soft tissue build-up of calcium (especially Matrix GLA Protein). Without adequate K2, the functioning of these proteins become impaired, and the risk of calcification increases. Thus, Vitamin K2 is extremely important not only in assisting proper calcium absorption, but also in the proper utilization of Vitamin D and guarding against calcification, and should therefore always be considered when supplementing D! This can also help explain why some people are able to more safely supplement high dose Vitamin D than others, without adverse consequences.
If you're wanting to raise your Vitamin D naturally, safe sun exposure is an excellent way, though that alone isn't always enough. This article has explained several other factors that need to be looked at that could contribute to a low level. A dietary focus should also be included. Some of the best dietary sources of Vitamin D include:
- cod liver oil...this is a particularly excellent source of Vitamin D because it is also paired with Vitamin A.
- fish - specifically salmon, sardines, herring, mackerel
- fish roe
- eggs - 1 egg contains roughly 10% DV. By the way, egg yolks also offer an excellent source of Vitamin K2!
- shiitake and button mushrooms - though a poorer source and ONLY if they have been grown in sunlight
- other sources include grass-fed butterfat and organ meats, cheese, and bone broth
Still scratching your head that the answer to raising your Vitamin D level could lie with magnesium. Consider the following:

"Hypomagnesemia impairs secretion of PTH and renders target organs refractory to PTH. Reduced secretion of PTH or impaired peripheral response to the hormone leads to low serum concentrations of 25(OH)D3. In addition, the hydroxylase enzyme 25-hydroxycholecalciferol-1-hydroxylase, which is responsible for production of the most active, hormonal form of vitamin D, calcitriol, requires magnesium as its cofactor. Consequently magnesium deficiency impairs calcitriol production." [10]
Or, from this study [11]:
"Intake of magnesium significantly interacted with intake of vitamin D in relation to risk of both vitamin D deficiency and insufficiency... findings indicate it is possible that magnesium intake alone or its interaction with vitamin D intake may contribute to vitamin D status."
Low Vitamin D may be an effect of illness or imbalance, rather than a cause.
Everyday, the public gets more and more confused and misled by the media and articles written by people and practitioners who have little understanding of the molecular effect of Vitamin D supplementation and its cascade of effects on a person's mineral profile; or by biased studies, or in some cases well-intentioned doctors who simply just weren't taught any different. We really have to start by asking if those who push high-dose Vitamin D supplementation and the importance of optimizing levels have ever bothered to look at a person's magnesium level first? Have they ever considered that many of the health effects of low Vitamin D may actually be a reflection of magnesium deficiency? Do they consider bio-individuality, which allows for some people to be able to tolerate higher doses (mega doses) of certain nutrients than what others can safely tolerate? Have they looked a kidney function? Or low boron? Have they considered that low 'Vitamin' D may actually be an effect of illness or imbalance rather than a cause, and that additional supplementation may be more so 'cause' than 'cure'. Very few people are standing up to write about this side of the story, and it is time that people come to understand (and take interest in) the effects of that which they put into their bodies, sold to them as 'healthy', but which may potentially be doing more harm than good.
"Vitamin D is far more often a cause, and not a cure for disease. And that discrepancy makes a world of difference. It is the difference between advising the public to supplement with vitamin D and telling people to avoid supplementation at all costs. It is the difference between preventing a disease and speeding its progression, the difference between fighting an epidemic of chronic disease, and watching more and more people fall ill every day. And it‘s a change that needs to happen right now."
~Amy Proal, Ph.D.
Further Exploration:
This article is meant as a primer to provide basic insight into Vitamin D's effect on one's mineral profile, and to start questioning the messages we are fed. For those who either question this information or desire to learn more at a molecular biology level, the links below will help, along with this brilliantly researched and supported paper:
https://d11n7da8rpqbjy.cloudfront.net/mineralhealth/31064032_1705201027219mb-0439-vit_D.pdf
These important Vitamin D concepts, and especially the interrelationship with minerals, is also one of the concepts taught even further within the Mineral Mastery education course.
UPDATES:
Update April 15, 2017
This recent New York Times article [16] provides an excellent explanation to some of the things mentioned above, including the history of how a few studies were able to dupe the public into believing this notion that everyone needs to supplement more Vitamin D.
Update April, 18, 2018
This Medscape article has just come out warning people (and prescribing physicians) of the dangers of excess Vitamin D. Meanwhile this study in the Journal of the American Osteopathic Association [18] as well as this review [19] have just come out that further explain the importance of magnesium for Vitamin D metabolism and usefulness. I've no doubt that in the years ahead, more and more 'news' stories will appear touting 'new evidence' suggesting Vitamin D supplementation may be harmful. The evidence however is not new. A handful of us have been teaching these warnings for years. It does seem though, slowly but surely, more and more people are waking up to this message that Vitamin D supplements can, in fact, be harmful.
Update August 2019
A recent study has shown the importance of glutathione in upregulating Vitamin D. They summarize that: "GSH status positively upregulates the bioavailability of 25(OH)VD, and that Vitamin D supplements widely consumed by the public are unlikely to be successful unless the GSH status is also corrected."[13] This, of course, makes sense, when we consider the vital importance of magnesium in supporting glutathione production. Much of the evidence and research provided by this article shines the spotlight on why magnesium is so important for improving Vitamin D status, and one more avenue of achieving that is via supporting GSH (which in turn supports Vitamin D bioavailability).
Update July 2022
The 3 year Calgary Vitamin D study examined the hypercalcemia effect of Vitamin D across 373 healthy participants. Participants were given a daily dose of either 400iu, 4000iu, or 10,000iu of Vitamin D daily. Hypercalcemia (total serum calcium > 2.55 mmol/l) occurred in 0%, 3% and 9% in the 400, 4000 and 10,000 iu/day groups, respectively [14].
Yet, people are continually convinced to be taking 5000iu, 10000iu or more, despite these known effects as we've been teaching here now for 6 years as of this update. Consider also that, due to blood's homeostatic nature, hypercalcemia is apt to much more quickly resolve itself than the soft tissue calcification (not as easily seen through blood but which can typically be evidenced through HTMA Testing) that occurs in the process.
It should not be a surprise at all, therefore, when a patient advised to take 150,000iu of Vitamin D, ends up in hospital, making the news. The patient had hypervitaminosis D (a growing trend) and hypercalcemia (in other words, high blood calcium and weakening of bone as calcium was being leached out). Of course, this is an extreme example of a mega-dose, but nonetheless it reflects the known dangerous effects of high-dose Vitamin D supplementation as this article explains, something patients should be informed of (and, of course, which practitioners ought to be better aware of).
REFERENCES
[1] http://www.medicinabiomolecular.com.br/biblioteca/pdfs/Biomolecular/mb-0439.pdf [Also Here]
[2] https://www.sciencealert.com/vitamin-d-tablets-may-be-worse-for-you-then-nothing-at-all
[3] http://pdf.usaid.gov/pdf_docs/Pnacr902.pdf [Also available at: http://tinyurl.com/acjazh3f ]
[4] https://www.westonaprice.org/health-topics/beyond-cholesterol/
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4160567/
[6] https://nap.nationalacademies.org/resource/13050/Vitamin-D-and-Calcium-2010-Report-Brief.pdf
[7] https://www.hoajonline.com/allergyasthma/2054-9873/2/2
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4160567/
[9] https://mpkb.org/home/pathogenesis/vitamind#fn__2
[10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4712861/
[11] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3765911/
[12] https://tinyurl.com/43ke7vke
[13] www.ncbi.nlm.nih.gov/pmc/articles/PMC6208166/
[14] https://academic.oup.com/jcem/article/105/4/1261/5634116
[15] https://web.archive.org/web/20130214152847/http://www2.macleans.ca/author/juliabelluz/
[16] www.nytimes.com/2017/04/10/health/vitamin-d-deficiency-supplements.html
[17] www.medscape.com/s/viewarticle/893083
[18] https://jom.osteopathic.org/abstract/role-of-magnesium-in-vitamin-d-activation-and-function/
[19] https://www.eurekalert.org/news-releases/891683
http://nutritionalbalancing.org/center/htma/science/articles/vitamin-d.php
http://bacteriality.com/2009/08/iom/
http://www.traceelements.com/Docs/News Jan-April 2008.pdf
http://naturopathconnect.com/articles/magnesium-calcium-potassium-vitamin-d-kerri-knox/
http://www.precisionnutrition.com/stop-vitamin-d
http://www.reuters.com/article/us-health-vitamind-supplements-idUSKBN19B2F0
http://theconversation.com/the-sun-goes-down-on-vitamin-d-why-i-changed-my-mind-about-this-celebrated-supplement-52725
http://jaoa.org/article.aspx?articleid=2673882
Follow Us
Copyright © 2014-2024 Integrative Health Coaching & Rick Fischer - All Rights Reserved.
All content and articles on this site may not be copied in whole or part without expressed written permission by Rick Fischer.


